Sleep & Blood Sugar – A Diabetic’s Guide to Better Rest
Summary:
Understanding the powerful link between sleep and blood sugar is crucial for individuals managing diabetes. Poor sleep increases insulin resistance, disrupts appetite hormones, and worsens glycemic control. Conversely, better rest enhances metabolic balance, supports emotional health, and reduces diabetes complications. This guide explores evidence-based research, common sleep challenges in diabetes (like nocturnal hypoglycemia and sleep apnea), and practical strategies—such as routine sleep schedules and stress reduction—for improved diabetic outcomes. By prioritizing quality sleep, diabetics can experience more stable blood sugar levels and a marked improvement in overall quality of life.
Introduction
Sleep is essential for overall wellness, but for people with diabetes, it is both more complex and more critical. This chronic condition affects how the body processes glucose, and sleep interruptions can directly influence blood sugar regulation. Unfortunately, diabetes can itself disrupt sleep, creating a challenging cycle that negatively affects health and well-being.
Many individuals with diabetes face issues such as insomnia, restless legs syndrome (RLS), and frequent nighttime trips to the bathroom. More serious challenges like nocturnal hypoglycemia or hyperglycemia can trigger regular awakenings that prevent deep, restorative sleep. Research shows even one night of reduced or poor-quality sleep can cause spikes in blood sugar, increased appetite, and enhanced insulin resistance the next day.
On the flip side, stable blood glucose levels promote quality sleep. Restorative sleep helps regulate hormones, improves insulin sensitivity, enhances mood, and helps control appetite—all indispensable elements in diabetes care. Yet, achieving the recommended 7–9 hours of quality sleep is often hindered by stress, inconsistent routines, diet choices, sedentary habits, or medication timing.
Good sleep is not just a comfort—it’s a therapeutic tool in diabetes management. In this guide, we explore how sleep affects blood sugar, how diabetes symptoms interfere with sleep, and the science-based methods that can improve sleep quality for diabetic patients. When managed effectively, sleep becomes a key pillar in strengthening physical resilience and boosting energy, performance, and metabolic health.
Sleep and Blood Sugar – What Research Shows
The connection between sleep deprivation and poor glucose control is well-proven. Clinical research confirms that a lack of sleep can impair how the body metabolizes glucose, reduce insulin sensitivity, and result in damaging hormonal shifts.
In a landmark study published in the Journal of Clinical Endocrinology & Metabolism, participants limited to just four hours of sleep per night over several days experienced a staggering 20–25% drop in insulin sensitivity. Even in healthy individuals, such a short period of sleep loss had a meaningful metabolic impact—imagine the effect on someone already managing type 1 or type 2 diabetes over the long term.
Similarly, an important study from Diabetes Care found that patients with type 2 diabetes who described poor sleep habits exhibited higher overall glucose levels and worse HbA1c measurements, which indicate long-term blood sugar control.
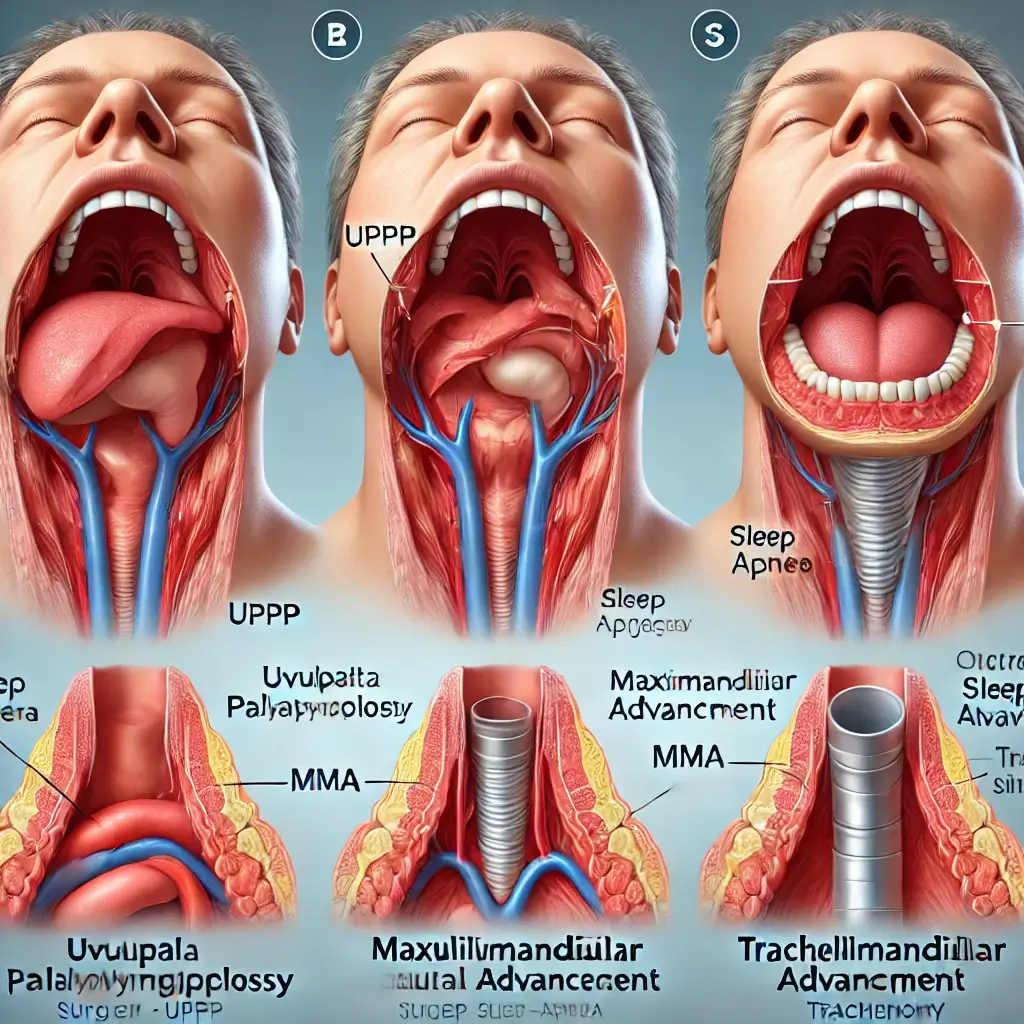
Obstructive Sleep Apnea (OSA), which causes interrupted breathing during sleep, plays a significant role in blood sugar irregularities. It’s especially prevalent among individuals with type 2 diabetes. Studies published in Current Diabetes Reports estimate 50–60% of people with type 2 diabetes also suffer from OSA. This overlap deepens blood sugar instability, increases the need for insulin, and makes sleep efficiency even worse over time.
Sleep issues are not restricted to adults. Children and adolescents with type 1 diabetes are also at risk. Research in Sleep Medicine found that teens with diabetes who had less sleep or fragmented rest saw greater glycemic variability and experienced more frequent nighttime hypoglycemic events. The impact wasn’t just physiological—it affected their academic performance, mental health, and capacity to self-manage their diabetes reliably.
Also worth noting, chronic sleep disruption contributes to diabetes complications like cardiovascular disease, diabetic neuropathy, and obesity. That’s because lack of sleep elevates cortisol levels (the stress hormone) and ghrelin (which stimulates appetite), while suppressing leptin (which tells you when you’re full). These hormonal shifts encourage overeating, promote weight gain, and elevate blood sugar levels—further aggravating insulin resistance.
This hormone cascade has been explored in studies published in PLOS Medicine, which showed that inadequate sleep correlates with higher BMI, cravings for unhealthy foods, and poor body composition—all influencing glycemic control.
The conclusion is clear: if blood sugar seems “unexplained” despite good diet and activity, it might be time to look at sleep quality. Healthcare providers are now encouraged to evaluate sleep patterns as part of comprehensive diabetic assessments, especially if applicable signs point to conditions like OSA or restless legs syndrome.
Conclusion
Sleep and blood sugar function as partners in an intricate feedback loop—especially for those with diabetes. Insufficient or poor sleep worsens insulin activity, appetite control, and hormonal balance, while healthy blood sugar regulation significantly improves the ability to achieve deep, restorative sleep.
Incorporating better sleep hygiene—like going to bed and waking at the same time daily, limiting screen time after dark, optimizing evening meals and medication, and managing emotional stress—can positively affect sleep quality and glucose regulation. Equally important is medical evaluation for sleep disorders such as sleep apnea or PLMD (Periodic Limb Movement Disorder), especially when typical diabetes interventions aren’t yielding expected results.
Sleep is not a luxury—it’s a cornerstone of chronic disease care. When optimized, it empowers diabetic individuals to better stabilize blood sugar, feel more energized, and reduce their risk for complications. Better sleep leads to better days—and better health outcomes.
References
- Spiegel, K., Leproult, R., & Van Cauter, E. (1999). Impact of sleep debt on metabolic and endocrine function. Journal of Clinical Endocrinology & Metabolism.
- Resnick, H.E., et al. (2003). Diabetes and Sleep Disturbances. Diabetes Care, 33(2), 414–420.
- Mokhlesi, B., et al. (2019). Obstructive Sleep Apnea and Glucose Metabolism. Current Diabetes Reports.
- Perfect, M.M., et al. (2012). Sleep disturbances in adolescents with type 1 diabetes. Sleep Medicine, 13(7), 820-828.
- Taheri, S., et al. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin and increased BMI. PLOS Medicine, 1(3): e62.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com